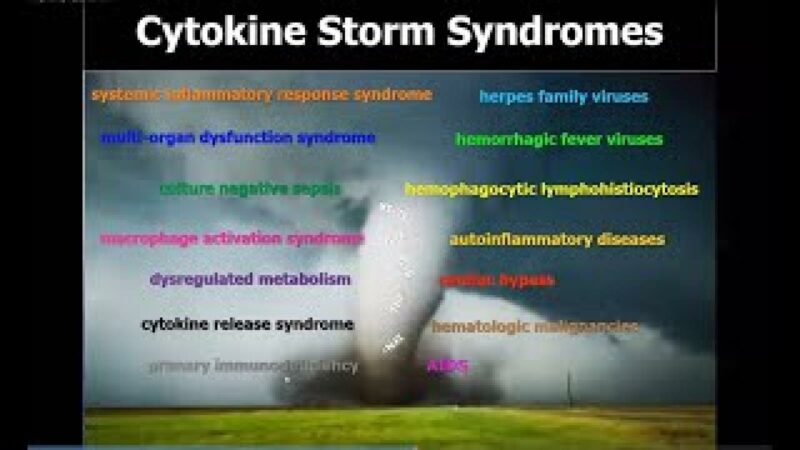
Macrophage activation syndrome (MAS) is a term commonly used by rheumatologists to describe a potentially life-threatening complication of systemic inflammatory disorders, most commonly occurring in people with systemic juvenile idiopathic arthritis (sJIA) and systemic lupus erythematosus (SLE). Time is the essence in the management of this condition as its associated mortality is very high. We need a therapy that will work rapidly and allow cessation of corticosteroid to improve long-term outcomes. Recently, interferon-gamma (IFNγ) has been implicated in the cytokine cascade during the cytokine storm in MAS.
At #ACR21, De Benedetti et al. (Abstr#L20) presented data from a pilot, open-label, single-arm study (NCT03311854) enrolling sJIA patients with MAS who had refractory disease to high dose corticosteroid. Emapalumab, anti-IFNγ monoclonal antibody was administered at 6 mg/kg and followed by 3 mg/kg every 3 days until day 15, and twice weekly until day 28. The duration of study was at least 8 weeks and all patients entered a 1-year follow-up study.
In this study, 14 patients were recruited of which some were also refractory to cyclosporine A or anakinra. The results were remarkable as all patients achieved complete response (11/14 within 8 weeks), as defined by resolution of signs and symptoms as adjudicated by the investigators AND normalisation of laboratory markers associated with MAS. At 8 weeks, all corticosteroid dose was reduced in all patients with 12/14 had ≥50% reduction from baseline. Emapalumab also demonstrated biological response through rapid reduction of CXCL9, a marker of IFNγ neutralisation. In terms of safety profile, Emapalumab was well tolerated. One cytomegalovirus reactivation case was reported as a serious event, possibly related to Emapalumab, and resolved with antiviral treatment. No death was reported.
Overall, data pertaining efficacy and safety of Emapalumab for the treatment of refractory MAS from this pilot study are promising.
So where do we go from here? Prior to licensing, this novel therapy should be evaluated in a Phase III randomised controlled trial. Recruitment of participants into the trial could be challenging since MAS is a rare complication. Hence, a multicentre collaboration is of paramount. Moreover, careful consideration is also needed to determine the comparison group; standard of care may be more suitable than placebo due to high mortality associated with MAS.
Related Content
-
February 25, 2016
Systemic juvenile idiopathic arthritis (SoJIA) is one of the most common underlying etiologies…
-
May 24, 2017
Adult-onset Still disease (AOSD) is usually regarded as an autoinflammatory disease, largely because…
-
January 1, 1970
Saturday's session on autoinflammatory syndromes featured Dr. Dan Kastner addressing - The Adult…
-
February 22, 2021
-
June 18, 2020
-
May 14, 2022
Vexed about VEXAS: Dr. Janet Pope https://youtu.be/hfm54-5IZLQ Diagnosing VEXAS Syndrome https://youtu.be/KOec2hXUBeU …