Your patient doesn’t meet criteria for Still’s disease (AOSD or sJIA), now what should you do or consider?
What you do or consider next can be addressed according to the stage of current disease: A) Hospitalized Febrile Disease, or B) Outpatient “Still’s” Disease.
- Hospitalized patients: the diagnosis of Still’s disease is easier and more certain if hospitalized for high fevers, multi-organ dysfunction and worrisome labs showing high inflammation. Moreover, more testing, imaging and consultations with specialists in the hospital can facilitate the correct diagnosis. Thus, if NOT diagnosed with Still’s disease after several days of evaluation in the hospital, a Still’s diagnosis is unlikely. Note: It is possible that patients in the first 6-12 weeks of symptoms may not have the requisite findings to make a Still’s diagnosis; thus, some patients can still be diagnosed with time (usually months).
- Outpatient “Still’s”: Many patients are often given a diagnosis of “Still’s” by clinicians who may not be familiar with this diagnosis or the diagnostic criteria. For those not in the hospital, a diagnosis of Still’s cannot be seriously considered without having the “Triad Symptoms” of 1) Daily Spiking Fevers >102F; 2) Intermittent JRA rash; and 3) Polyarthritis. Moreover, it’s very unlikely to have this diagnosis if patients have: Fevers <101F, rash on the face, WBC < 3.0, only one swollen joint, age over 60 yrs., and a good response to prednisone 10-20 mg per day.
Concerns: Not meeting “criteria” for Still’s disease, often leaves the patient concerned about:
- How can I get an accurate diagnosis?
- Who is the best doctor or center to evaluate my condition? Find a physician.
- What tests or treatments should be tried?
Questions and Future Considerations:
- Can a patient have Still’s disease but not meet criteria?
- Yes, but unlikely. Meeting criteria (according to the Still’s disease calculator) greatly increases the likelihood it is Still’s disease.
- There is no test that is truly diagnostic of Still’s disease.
- Still’s disease is a syndrome, meaning that the diagnosis is based on excluding other causes (that may look like Still’s) and having typical symptoms, findings, and lab results compatible with a Still’s diagnosis.
- Consult with a Still’s expert who can guide your search for a diagnosis, treat you, and see if your treatment responses can help define your diagnosis.
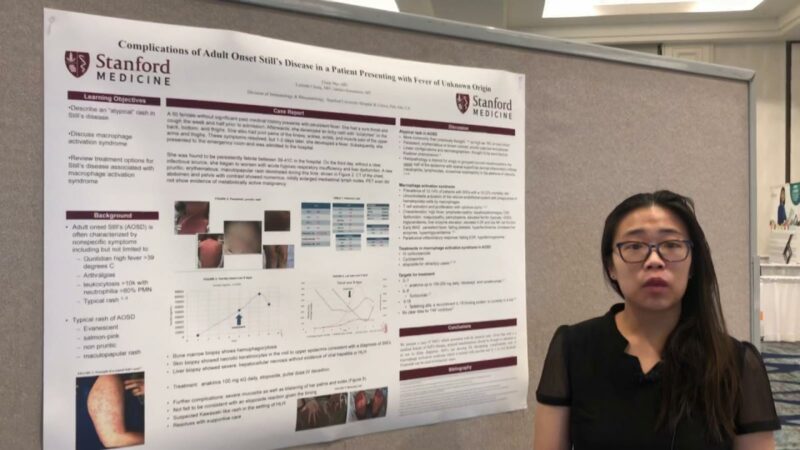
- What other diagnoses are often confused with Still’s disease?
- Other autoinflammatory disorders
- Adults: FMF, Schnitzler’s syndrome, Muckle-Well’s syndrome, TRAPS, cyclic neutropenia
- Children: CAPS, FACS, Muckle-Wells syndrome, FMF, TRAPS
- Autoimmune diseases with fevers: Lupus, inflammatory myositis (dermatomyositis), MCTD, Sweet’s syndrome, Kikuchi’s disease, Behcet’s syndrome
- Infections: sepsis, pneumonia, bacterial endocarditis, bacterial pleuritis or pericarditis, tuberculosis, fungal infections
- Malignancies: leukemia, lymphoma
- Other autoinflammatory disorders
- What if the patient had a good or great response to “steroids”?
- Unfortunately, steroids nonspecifically improve inflammation and pain, thus making most people feel better, regardless of diagnosis. Hence, a good steroid response is common but not specific to the quest for an accurate diagnosis. Importantly, chronic steroid use is dangerous, especially at doses greater than 10 mg daily (prednisone equivalent).
- What if the patient had a good or great response to a “biologic” drug (e.g., anakinra, canakinumab, tocilizumab, sarilumab)?
- This is potentially helpful in establishing the diagnosis
- But, a great response to these biologics is not unique or specific to Still’s disease and may also be seen in other conditions, like infection and other febrile or autoinflammatory disorders.
- With very high inflammation tests (e.g., WBC, ESR, CRP, Ferritin), what could this be if not Still’s disease? (See Lab & Diagnostic Tests)
- High White Blood Cell (WBC) counts: normal values are more than 3,000 and less than 10,000 cells/mm3.
- WBC counts greater than 15,000 can be seen in acute and chronic infections, other inflammatory and autoinflammatory disorders, and some cancers.
- High ESR (erythrocyte sedimentation rate or “sed rate”)
- Normal is 0-20 mm/Hr.
- 20-50 would be a low-level elevation that is not diagnostic and seen in MANY conditions
- Greater than 50 is seen with inflammation, infection, pregnancy, anemia, kidney disease, chronic lung disease, autoinflammatory (FMF, TRAPS) and autoimmune diseases (lupus or rheumatoid arthritis)
- Greater than 100 is seen in fewer conditions including Still’s disease, other autoinflammatory diseases, infection, chronic infections, vasculitis, macrophage activation syndrome
- For adults, a Sed Rate (ESR) that is much higher than your age (yrs.) is potentially worrisome and should be discussed with your medical provider.
- High White Blood Cell (WBC) counts: normal values are more than 3,000 and less than 10,000 cells/mm3.
- Up to 90% of patients with Still’s disease will have an elevated CRP > 1.0 mg/dl (or 10 mg/L). CRP may also be elevated with infection, autoimmune disease (Lupus, RA) and other chronic conditions (like kidney or lung disease).
- High Ferritin levels (normal is up to 150 ng/mL). Half of patients with Still’s disease will have an elevated ferritin (iron level), but alone, this is poorly predictive of Still’s disease. Extreme elevation of Ferritin (more than 2000) is more suggestive of Still’s disease. But extreme elevation of ferritin may also be seen in other disorders, including macrophage activation syndrome, HLH (hemophagocytic-lymphohistiocytosis), major liver injury/disease, severe COVID-19 and other severe infections, sepsis, and iron overload disorders (multiple blood transfusions or hemochromatosis)
- With unexplained (high) fevers, genetic and other tests may be indicated:
- Genetic testing: can be ordered to diagnose genetically based fever disorders or autoinflammatory diseases via:
- Autoinflammatory gene panels (see Invitae.com)
- Whole exome sequencing
- Such testing is often expensive, not routinely available, must be specially ordered and take weeks to receive results
- What Other Lab Tests should be considered (if not already done)?
- Hepatitis tests (for hepatitis B or hepatitis C), tests for TB (Quantiferon-TB or T-Spot.TB tests), blood or urine tests for chronic infection, ferritin, ANA, ANCA, HLA-B27, urinalysis, muscle enzymes (including CK and aldolase)
- Genetic testing: can be ordered to diagnose genetically based fever disorders or autoinflammatory diseases via:
- Should steroids be subscribed to see if they’ll help? Would this confirm the diagnosis of Still’s disease?
- NO!
- Steroids should not be given without a firm or likely diagnosis of Still’s disease. There are several serious problems with steroid use:
- Steroids make everyone feel better, regardless of the underlying diagnosis.
- Steroids are hard to stop, once you’ve started and feel better on steroids.
- Steroids are acutely/quickly wonderful but chronically dangerous and hazardous.
- They cause infections, ulcers, fractures, cataracts, diabetes, anxiety, insomnia, weakness, bruising, bleeding, thin skin and much more.
- What about “active disease” according to the “Disease Activity Calculator” but not Still’s according to the Still’s Diagnosis Calculator?
- Most patients with active Still’s disease will have a score of 4 or higher. While lower scores suggest a diagnosis other than Still’s disease, scores between 4-7 can be seen with other diseases.
Related Content
-
January 1, 1970
A small retrospective study suggests that patients with difficult to treat adult-onset Still's…
-
February 17, 2020
-
May 14, 2022
Emapalumab Treatment in Macrophage Activation Syndrome: Dr. Fabrizio De Benedetti https://youtu.be/yHBRXphEhe0 Macrophage…
-
November 6, 2021
-
July 29, 2022
QD197 - Still's (or Not) NEJM CPC https://youtu.be/_xnCaxeqidwQD198 - Still's (or Not) with…
-
January 1, 1970
Still's disease is an autoinflammatory disease characterized by spiking fever, rash, polyarthralgia, sore…