Adult onset Still’s disease (AOSD) is a little bit of both: it can be a diagnostic conundrum and it can have complications.
AOSD is sometimes mentioned in movies or medical shows, likely because it’s an extremely rare disease with an incidence of 16 per 10 million. Further, for the most part it has a bimodal distribution: one peak between ages 15 to 25 and the second between ages 36 to 46 years. Some studies do report patients diagnosed above the age of 60.
Many clinicians may not have seen a case of AOSD during training, which overall leads to several delays in referrals and appropriate diagnosis for AOSD patients. AOSD is an autoinflammatory disease where innate immunity plays a primary role and is characterized by seemingly unprovoked inflammation, but without the high-titer autoantibodies or antigen specific T cells seen in autoimmune diseases.
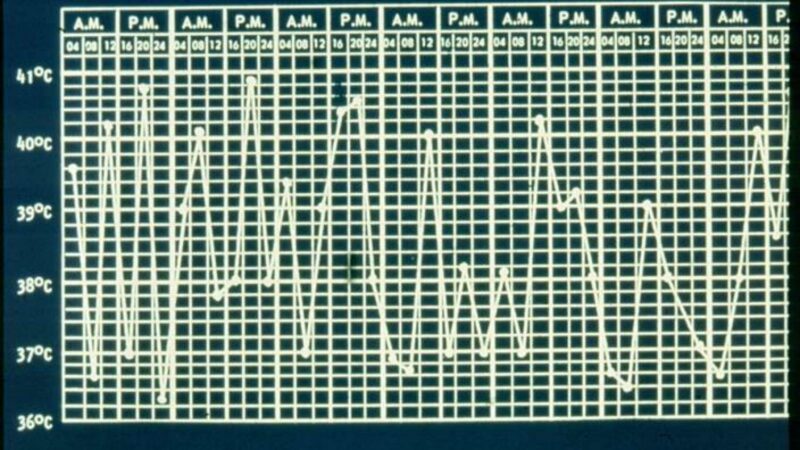
The common clinical features include spiking fever, arthralgia, myalgia, maculopapular rash, and pharyngitis. Other features include – elevated liver enzymes, lymphadenopathy, hepatosplenomegaly, and serositis. A lot of infectious diseases, including viral illnesses may present like this and are much more common than Still’s disease. Differential diagnosis also include malignancies, adverse drug reaction or other rheumatic diseases that may present with similar findings.
All of the criteria for AOSD, including Yamaguchi’s original criteria, do require that other differential diagnosis are ruled out. AOSD can present in many patterns – monocyclic pattern (single episode), polycyclic pattern (multiple flares lasting for a 1 year or longer, alternating with remissions) or chronic pattern (active with polyarticular disease).
While serum ferritin is elevated in most patients, it may not be the case in all patients. Glycosylated ferritin, C-reactive protein, calprotectin, serum Amyloid A are commercially available biomarkers that can help clinicians with the diagnosis. Biomarkers in research studies which may not be easily accessible for clinical care include – serum cytokine levels (IL-1, IL-6, IL-18), chemokines such as CXC-chemokine ligands 10 and 13, advanced glycation end products (AGEs), soluble receptor for AGEs (sRAGE). The lack of serologic biomarker, wide range of clinical presentation along the rarity of AOSD often result in a significant delay in diagnosis.
Sometimes patients with AOSD may first present to the hospital with life threatening complications such as Macrophage Activation Syndrome (MAS), fulminant hepatitis, myocarditis, acute respiratory distress syndrome, disseminated intravascular coagulopathy, pulmonary artery hypertension, diffuse alveolar hemorrhage, and thrombotic thrombocytopenia purpura. Early diagnosis and treatment are a key in prevention of worsening complications and mortality. Usually after infectious etiologies are ruled out, these patients are often treated with high dose steroids and immunosuppressants.
IL-1 therapy has now become the mainstay in chronic AOSD care, but patients with some of these complications may require different regiments. For example, some patients with MAS require regiments with etoposide and cyclosporine as immunosuppressants. These patients are best managed by a multidisciplinary team including intensivists, hematology, pulmonary etc. with rheumatology playing an integral role.
I believe raising the awareness of this complex disease in local medical communities will facilitate appropriate referrals and timely diagnosis of AOSD patients and improve the outcomes in adults who were seemingly healthy before the onset of AOSD symptoms.
Related Content
-
May 24, 2017
Adult-onset Still disease (AOSD) is usually regarded as an autoinflammatory disease, largely because…
-
March 12, 2020
An Italian study examined the outcomes in adult onset Still's disease (AOSD) based…
-
January 1, 1970
Still's disease is an autoinflammatory disease characterized by spiking fever, rash, polyarthralgia, sore…
-
February 25, 2020
Rheumatology has a comprehensive overview of methotrexate (MTX) and the risk of lung injury,…
-
January 1, 1970
A small retrospective study suggests that patients with difficult to treat adult-onset Still's…
-
November 26, 2019
A disease you’ve never heard of is becoming increasingly common and carries a…