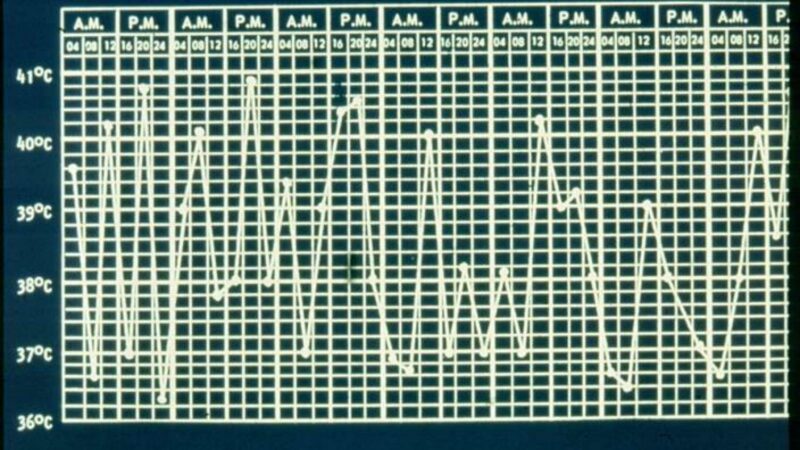
Differentiation between a flare of disease and infection in patients with autoinflammatory (AI) conditions, where fever is the hallmark, can be extremely difficult. Promptly distinguishing between the two is of extreme importance in AI patients with compromised immune systems, often receiving immunosuppressive therapy. Few studies have evaluated potential differentiators; and having such tools would meet a huge unmet need.
A cross-sectional study outlined in abstract # 0252 makes an attempt in identifying laboratory parameters that could distinguish disease flare from infection in febrile patients with systemic-onset juvenile idiopathic arthritis (SJIA).
The comparative cohort included SJIA patients with confirmed infection (40 patients, 76.9%) SJIA flare (12 patients, 23.1%). Unfortunately, none of the conventional inflammatory markers such as CRP, ferritin and procalcitonin differentiated between groups.
More valuable were the clinical parameters (quotidian fever, evanescent maculopapular rash and joint symptoms) that were more distinguishing and statistically significant (p value: < 0.05). Moreover, procalcitonin levels can be of some utility in predicting macrophage activation syndrome (MAS) as levels greater than 0.95 ng/mL served as a reliable predictor of MAS.
Another single center retrospective analysis of extremely elevated ESR levels in patients with rheumatic disease (abstract #1094) evaluated 311 patients with high ESR≥100 mm/h and rheumatic disease. The most common disorders in this study were RA, SpA, JIA, vasculitis, SLE, FMF, AOSD, SSc, Sjogren’s syndrome and sarcoidosis. Several cases of Behcet’s, retroperitoneal fibrosis and PMR were represented in the infection group. Thrombocyte counts, MCV, albumin and total protein were significantly lower in infection groups and favored infection over disease flare up, particularly if coupled with extremely high ESR.
While none of the studies identifies one perfect laboratory marker which could make decision easy for a clinician, using multiple markers in combination and pairing with clinical presentation may guide one in the right direction and best diagnosis.
Meanwhile, the search for an ideal diagnostic tool continues.
Related Content
-
May 24, 2017
Adult-onset Still disease (AOSD) is usually regarded as an autoinflammatory disease, largely because…
-
March 12, 2020
An Italian study examined the outcomes in adult onset Still's disease (AOSD) based…
-
November 26, 2019
A disease you’ve never heard of is becoming increasingly common and carries a…
-
August 20, 2020
You can reduce - but not stop - canakinumab therapy in patients who…
-
November 10, 2020
With broader awareness about the disease state, early diagnosis and treatment in autoinflammatory…
-
May 14, 2022
Featuring Drs. Jack Cush, Bella Mehta, Olga Petryna, and Michael Ombrello